Pediatric tumors

Description
As for adult cancers, pediatric tumors can be treated by surgery, chemotherapy and / or radiotherapy according to the type of cancer with high cure rates.
About a thousand children receive radiotherapy in France each year. For 300 to 500 of them proton therapy could be discussed.
Treatment procedure
Consultation, treatment, multidisciplinary meeting
Each patient will be seen in consultation by the radiation oncologist to collect all the clinical, radiological and histological information and then present the case in multidisciplinary meeting to validate or not the indication for proton therapy.
The case can be discussed in a multidisciplinary meeting before the consultation with the radiation therapist to speed up procedures and if all the elements of the case are sufficient to make it possible.
Besides obvious clinical indication and prior consultation, a computer simulation of the treatment can be performed to assess the magnitude of the benefit of the proton treatment over a conventional radiotherapy by photons or electrons. Indeed, it may be that conventional treatment is appropriate and that proton therapy is not necessary.
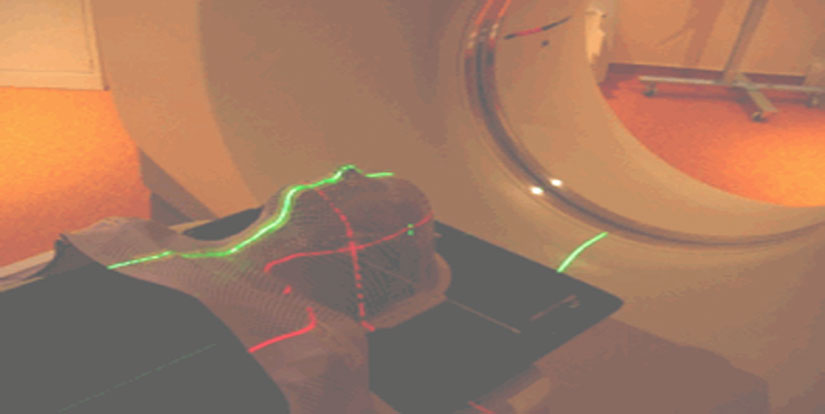
A simulation CT is performed to collect the images on which the zones to treat and to avoid will be delineated. A mask is sometimes used to immobilize head lesions as to always treat them in the same position.
For children, an anesthesia consultation with parents / guardians and the child will be scheduled in the city of origin or in Nice if anesthesia is required for all treatment steps. The day of the consultation with the radiation oncologist the entire treatment will be presented to the child in a playful way (model, treatment room visit). In case of chemotherapy, a consultation will take place in Nice and/ or the city of origin to implement chemotherapy if indicated during radiotherapy.
Treatment initiation
The total dose of irradiation given is divided into multiple small doses of 1.8 to 2 Gy most of the time. These doses are delivered daily (once daily) except weekends and holidays. The total irradiation time is from several weeks (1 to 1 month and a half). The patient is seen once a week by a medical doctor, or more if necessary, to detect and treat the symptoms related to radiation. All patients will be seen by a doctor (in Nice or in the referral center) several weeks after radiation to monitor the short-term tolerance of treatment.
Preparation for pediatric proton therapy
It is important to prepare your child to proton therapy because of anxiety that can appear both to your child and yourself by the treatment and the distance from your home. It is necessary to deliver clear, understandable and age-appropriate information for your child. Children fears depend on their age, personality and the treatment itself.
Usually, young children are more afraid of being separated from their parents while older children are more afraid of pain. Some teenagers do not just fear pain but also have difficulty recognizing that they are afraid of pain. They may also be embarrassed if the treatments involve the genitals.
Children who need a treatment under general anesthesia may not understand “special” sleep associated with anesthesia and they need to be reassured. Older children and teenagers may also worry how they will recover after the session. It is important to discuss, acknowledge the fears and feelings of your child. This is especially true if your child has a preexisting fear or a bad experience with treatments that have not been well tolerated. If your child is in this case, he can benefit from working with the psychologist of our team.
Parents preparation
Some parents think that they should not speak of the treatment and its duration. However, children need a clear and honest information.
Many children can deal with the pain, machine noise or uncomfortable positions when they know what is going to happen and how long it will last. Saying this information in advance can help your child stay calm during the treatment session.Our team and our psychologist can help you find the right words to explain treatments and help your child understand what is happening
It is natural to be upset if your child is anxious or suffering. Take the time you need to learn about treatment with irradiation and prepare yourself emotionally. Knowing what it takes will help you to remain calm and support your child. Do not hesitate to ask what part of the treatment can be impressive and what measures will be taken to improve comfort. Our team and our psychologist will help you better understand the treatment. In some cases, you will be able to stay with your child in the treatment room just before the actual treatment phase.
Children prepration
Children older than 2 years should have as much information about the treatment as they ask for. Of course, the conversations you have with your child must be related to age and level of understanding of your child. Be honest and open but avoid too scary graphic descriptions. Learn to recognize the signals as when your child has received sufficient information. Our team and our psychologist can offer to your child, if he wants to play, to reproduce the treatment on a model with a teddy bear or a doll. At home, you can rehearse the treatment with your child, taking into account how long the treatment will occur and the position in which your child is to be held. It is important, wherever possible, to understand that children rely on the support of their parents and remain with them as possible.
During treatment
You and your child can set up a calendar with days of treatment and determine for example who will accompany him during the irradiation sessions. Be sure to discuss your agenda with a care team member to ensure it does not interfere with treatment.
Here are some tips to help your child stay as calm as possible during the irradiation sessions: bring their own music on CD, DVD or a book on CD to listen during treatment (our room is equipped with multimedia), give your child an achievable goal, tell your child that it’s okay to cry but his work consists to stay calm and still during the treatment.
After the treatment you may notice changes in your child’s behavior. Some may have a regression by acting younger than their age. Others will need you to be closer to them and will be separated from you more difficultly. These reactions are common and usually go away with time. We must recognize the frustrations related to the treatment of your child but it is important to continue to offer activities adapted to his age, to remain consistent with the routine and regular behavior of your family.
Key messages:
– Preparation for irradiation can help reduce stress and anxiety for both parents and children
– You can help your child by adapting information about treatment depending on age and level of comprehension of your child.
– Our team and our psychologist will help you.
Side effects
The side effects depend on the treated area and the sensitivity of each, which is not predictable. Some patients will have no side effects, others will. The lists below are not exhaustive and side effects may vary according to size and position of the tumor. These variations are explained by the radiation oncologist during the consultation and the occurrence of side effects can be properly assessed after completion of dosimetry.
For tumors of the head:
– During radiation: hair loss, fatigue, nausea, headache, rarely seizure or disorders of sensation/motor skills generally reversible and manageable,
– In the months and years after: Possible deficits in hormones, minimal cognitive deficits, very rare vascular disorders or radiation-induced cancers whose risk is decreased with the use of proton therapy.
For other locations, the set of underlying symptoms can appear both during radiation long after:
– Tumors close to the lungs and esophagus: fatigue, difficulty eating (pain, blockage) with a possible weight loss, cough, spitum, breathing difficulties of minimal intensity and reversible
– Abdominal tumors: asthenia, nausea, diarrhea.
– Tumors of the pelvis: burning sensation during urination, increased frequency of urination, anal pain, diarrhea,
– Tumors close to the skin: skin inflammation with redness, pain, sometimes ulcerations

 English
English Deutsch
Deutsch Italiano
Italiano Français
Français Русский
Русский